Medicine
 · From 5th to 6th in age-standardized YLD.
· From 5th to 6th in age-standardized YLD.
- Rosiglitazone And The "holy Grail"
. On Wednesday (July 14, 2010), the FDA advisory council looking at whether to ban rosiglitazone (Avandia ®), a drug for the treatment of diabetes that has been found to significantly increase the rate of heart attacks (MIs) decided to not ban it, but...
- Health Outcomes: The Interaction Of Class And Health Behaviors
. I have recently discussed (Poverty, Primary Care and the Cost of Medical Care, February 10, 2010) the “Whitehall Studies” conducted by Sir Michael Marmot and colleagues that “demonstrate that there is a more or less linear correlation between...
- Actual Causes Of Death In The U.s.: Not What You Think
Any standard public health or medical school prevention text includes (or ought to include) some version of the figure below, which illustrates that the leading causes of death in the U.S. at the turn of the century (heart disease, cancer, stroke) were...
- Actual Causes Of Death In The U.s.: Not What You Think
Any standard public health or medical school prevention text includes (or ought to include) some version of the figure below, which illustrates that the leading causes of death in the U.S. at the turn of the century (heart disease, cancer, stroke) were...
- Guest Blog: Avoiding "excess Deaths"
Dr. Ed Pullen is a family physician who practices at Sound Family Medicine in Puyallup, WA. The following piece is excerpted from a previously published post on his blog, DrPullen.com. ** "Excess death" or excess mortality is defined by the free medical...
Medicine
The State of US Health: improved over 20 years, but not nearly enough
An enormous, and enormously important, study was recently published online-ahead-of-print in JAMA describing the state of health in the US and comparing it that in other 33 “developed” countries in the Organization for Economic Cooperation and Development (OECD). “The State of US Health, 1990-2010: Burden of Diseases, Injuries, and Risk Factors”[1]was written by the members of the US Burden of Disease Collaboration, an enormous group of population-health scholars from institutions across the country and a few from other parts of the world. The methods used are incredibly complex; indeed editorialist and President of the Institute of Medicine (IOM) Harvey V. Fineberg, MD PhD (“The State of Health in the United States”)[2]calls it “…an arcane and complex process, and despite the authors’ best efforts to explain their methods and make data available, few readers will fully understand how the results are derived.” Nonetheless, the findings are incredibly important.
Here are the main results:
Since 1990, the health status of the US has improved in most areas.
· Average life expectancy has increased, from 75.2 to 78.2 years;
· Healthy life expectancy (HALE) has increased, from 65.8 to 68.1 years;
These are good things; that is, they are moving in the right direction. However, they are moving in the right direction more slowly than in the other OECD countries, so that, since 1990, the US rank for life expectancy (at birth) has dropped from 20th to 27th among these 34 countries, and the HALE has dropped from 14th to 26th!
A few more terms, not that hard to understand: Life expectancy is decreased by the years of life lost through premature (age-standardized) death due to disease or injury (YLL). The difference between absolute life expectancy and HALE is the number of years lived with disability (YLD). The sum of YLL and YLD is expressed as disability-adjusted life years (DALY), kind of the complement of HALE. That is, the lower the DALY, the fewer years of life have been either lost to premature death or lived with disability. From 1990, the US rank among the OECD countries has dropped in all these areas:
· From 18th to 27th in age-standardized death rate;
· From 23rd to 28th in YLL;
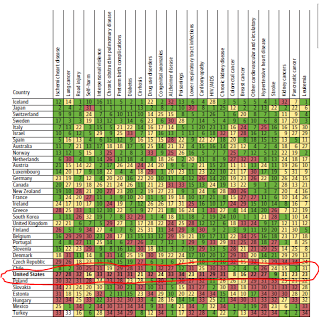
These are not good things. The table indicates, for each of the 34 countries, the rank for YLL for each of 25 conditions: green means significantly better than the mean, yellow about the mean, and red significantly worse. The US is green in only one (stroke), and is red in 15!
The other important thing done by the study’s authors was to look at risk factors for YLL and YLD in the US. As Fineberg explains, this is a complicated and difficult task,”…attempting to estimate the contribution of each risk factor to premature death.” It is easier to measure mortality (death) than morbidity (disability), but it is important because, as noted in the abstract, “As the US population has aged, YLDs have comprised a larger share of DALYs than YLLs.” That is, years lived with disability exceeds years of life lost from treatable disease. This makes sense; as we have developed increasingly sophisticated (and costly) high-tech interventions to prevent death (discussed by me, for example, in Primary Care Contributes More than Money..., June 2, 2013), we have increased the number of years that people are kept alive but suffering from the symptoms and complications of their diseases. The article's abstract contains 4 sentences that describe this:
- “The diseases and injuries with the largest number of YLLs in 2010 were ischemic heart disease, lung cancer, stroke, chronic obstructive pulmonary disease, and road injury.
- Age-standardized YLL rates increased for Alzheimer disease, drug use disorders, chronic kidney disease, kidney cancer, and falls.
- The diseases with the largest number of YLDs in 2010 were low back pain, major depressive disorder, other musculoskeletal disorders, neck pain, and anxiety disorders….
- The leading risk factors related to DALYs were dietary risks, tobacco smoking, high body mass index, high blood pressure, high fasting plasma glucose, physical inactivity, and alcohol use.”
The largest number of YLLs were caused by the “traditional” chronic diseases, while most of the conditions that increased YLL over the last 20 years were those that one would expect to increase as we keep people alive longer, particularly Alzheimer’s disease, chronic kidney disease, falls, and drug use disorders (which includes not just “illicit” or “illegal” drug use, but those taking prescription drugs, in particular for chronic pain – which comprise a large proportion of the diseases that have the largest number of YLDs -- back pain, other musculoskeletal disorders, neck pain).
These findings should guide our population/public health interventions. And the leading risk factors for DALYs are not surprising; they are the ones that we hear about all the time: dietary risks, tobacco smoking, high body mass index, high blood pressure, high fasting plasma glucose, physical inactivity, and alcohol use. These are the very areas, in fact, where most population/public health programs are currently focused. However, when it comes to public policy, laws, and spending money to try to solve the problems, we are woefully deficient in the US. There has been some success in regulation of smoking in public places although not without significant resistance from those who profit from tobacco, including the tobacco industry, tobacco retailers, and clubs and casinos; indeed the public smoking ban passed in my state of Kansas a few years ago is being threatened with repeal. Public interventions in the other areas have had much greater opposition (see New York City’s efforts to limit portion size of sugar-filled soft drinks) or non-existent.
What is popular is victim-blaming, telling people who are overweight, inactive, smokers, drinkers, and victims of diabetes or hypertension to “clean up their acts”, to stop, to lose weight, to adopt healthy habits. Of course, these would be good, and we see increasing numbers of individuals doing so. However, the success rate is much higher among groups with higher income and higher educational levels, which must mean something. It could be that they know that smoking, obesity, inactivity, drinking, drugs, and not taking medicine for diabetes and high blood pressure are bad for you, while poorer people don’t. That, however, is hard to imagine. It is more likely due to their greater level of resources to try to address these problems, social support for healthful behaviors (including jobs), and access to health care. In addition, the same interests that lobby against regulation of smoking, unhealthy foods and alcohol are heavily advertising these same substances in the least-advantaged communities.
The “social determinants of health” are at play here; not only access to health care, but safe communities, stable housing, education, and prospects for jobs – the very things that national and often state policymakers seem to be least willing to fund, and the areas that other OECD countries often do fund. As discussed by Bradley and Taylor in their book and NY Times Op-ed “To fix health care, help the poor” and by me in my post from December 18, 2011, “To improve health the US must spend more on social services”, the US stands out among OECD countries in that the vast majority of its combined health and social services spending is on medical care. This helps explain both our decrease in YLL from treatable but essentially end-stage medical conditions and our increase in YLD and in risk factors for chronic disease, because, as Bob Bowman described so well in “Moving to Recovery By Design”, June 22, 2013,we do not treat the “upstream” circumstances of people’s lives that lead to “downstream” disability and death. Even the US Burden of Diseases Collaborators have left out discussion of the social issues, which is perhaps on purpose but did not escape Fineberg’s notice: “The most glaring omission in the assessment of risk factors, as the authors acknowledge, is the role of social factors such as income and inequality as a risk of premature death and disability.” It is, as he acknowledges, harder to measure, but that scarcely decreases its relevance.
It is not about the money. We have the money. It is, as I have said before, about the will. About the will of politicians, who are ideologically committed to the principle that the only ones who really deserve government assistance are the largest corporations and wealthiest individuals and have, as Charles Blow has said (“Resonance Resistant”, May 18, 2013), a gag reflex to the word “social”, but also the will of the American people who often seem to value high-cost, high-tech care at the end of life more than healthful nurturing of people at its beginning.
27thin age-standardized death rate? 28th in years of life lost? Come on! Where is that old American competitive spirit? We can do it. We know that. Now, we must do it!
[1] US Burden of Disease Collaborators, “The state of US health 1990-2010”, JAMA. 2013;():. doi:10.1001/jama.2013.13805. Published online July 10, 2013.
[2]Fineberg HV, “The State of health in the United States”, JAMA. 2013;():-. doi:10.1001/jama.2013.13809, published online July 10, 2013.
- Rosiglitazone And The "holy Grail"
. On Wednesday (July 14, 2010), the FDA advisory council looking at whether to ban rosiglitazone (Avandia ®), a drug for the treatment of diabetes that has been found to significantly increase the rate of heart attacks (MIs) decided to not ban it, but...
- Health Outcomes: The Interaction Of Class And Health Behaviors
. I have recently discussed (Poverty, Primary Care and the Cost of Medical Care, February 10, 2010) the “Whitehall Studies” conducted by Sir Michael Marmot and colleagues that “demonstrate that there is a more or less linear correlation between...
- Actual Causes Of Death In The U.s.: Not What You Think
Any standard public health or medical school prevention text includes (or ought to include) some version of the figure below, which illustrates that the leading causes of death in the U.S. at the turn of the century (heart disease, cancer, stroke) were...
- Actual Causes Of Death In The U.s.: Not What You Think
Any standard public health or medical school prevention text includes (or ought to include) some version of the figure below, which illustrates that the leading causes of death in the U.S. at the turn of the century (heart disease, cancer, stroke) were...
- Guest Blog: Avoiding "excess Deaths"
Dr. Ed Pullen is a family physician who practices at Sound Family Medicine in Puyallup, WA. The following piece is excerpted from a previously published post on his blog, DrPullen.com. ** "Excess death" or excess mortality is defined by the free medical...
