Medicine
.
In a recent report from the University of Washington’s WWAMI Rural Research Center, “Family Medicine Residency Training in Rural Locations”,[1] Chen et. al. repeat their 2000 study of rural training in the US. They note that this is very important given the health needs of the American people, 20% of whom live in rural areas, most of which are underserved given the less than 9% of doctors who practice there (Primary Care and Rural Areas, April 28, 2010; Medicare Costs in Rural America: A case of reaping what we haven't sown?, March 26, 2009). Most rural training is of family doctors, but a majority of it comes from urban programs.
How is this so? This is because over 90% of the family medicine residency programs in the nation are located in urban areas, and only 7% in “large rural areas”; it is very hard to have a program entirely in a “small rural area” as the requirements for family medicine training include a great deal of time spent in the hospital and working with other specialists. Nonetheless, the authors surveys discovered that nearly half of the family medicine programs felt that training rural doctors was an important part of their mission.
From the Executive Summary: “Rural residency programs provided a higher proportion of rural training than urban programs,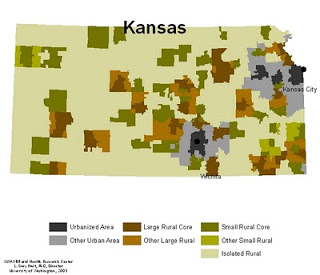 but because more programs were in urban settings, there was more rural training in urban than rural programs. Overall, 15% of respondents had a formal RTT [rural training track]; of these, 61% were in rural and 10% in urban programs. Rural residency programs conducted 83% of all rural residency training in RUCA[2]-defined rural areas. Comparing the 2000 and 2007 surveys, rural training increased from 372 to 408 FTEs, but rural training in urban programs declined from 186 to 79 FTEs, resulting in an overall decrease in the amount of rural-focused family medicine training.” See figure for example of a “RUCA map” in a state (Kansas) with a high percentage of “isolated rural” areas; Other states (say, New Jersey) look different!
but because more programs were in urban settings, there was more rural training in urban than rural programs. Overall, 15% of respondents had a formal RTT [rural training track]; of these, 61% were in rural and 10% in urban programs. Rural residency programs conducted 83% of all rural residency training in RUCA[2]-defined rural areas. Comparing the 2000 and 2007 surveys, rural training increased from 372 to 408 FTEs, but rural training in urban programs declined from 186 to 79 FTEs, resulting in an overall decrease in the amount of rural-focused family medicine training.” See figure for example of a “RUCA map” in a state (Kansas) with a high percentage of “isolated rural” areas; Other states (say, New Jersey) look different!
The authors found that while virtually all (99.9%) of the training FTEs reported as rural in rural programs in fact occurred in rural (RUCA-defined) areas, only 21.7% of those reported by urban programs were in such areas. The net result was that only 7.3% of family medicine residency training FTEs are in rural areas, with 83% of these conducted by rural programs. Interestingly, to me, a higher percentage of urban programs listed rural training as “very important” (45.3%) than listed urban (underserved) training (40.4%).
The authors discuss the policy implications of this situation, including the possible impact of several components of the ACA health reform law that encourage training in rural areas. An important one has to do with Medicare funding of GME (residency) positions, the arcane but major source of funding for such training (Funding Graduate Medical Education, May 25, 2009; Public Law 111-148, Sect 5506, p 661). The change would make it easier for non-hospital sponsors of training (such as community health centers, an area the authors have also written about[3]) to receive this funding (Public Law 111-148, Sect 5508, p.668). The law – and policy – also favors redistribution of unfilled GME spots to rural hospitals. However, there are counterpressures: many big urban hospital training sites are “over their cap”, meaning they have more residency positions than are funded by Medicare. In these cases, the hospital, or another entity, funds the positions; these are virtually always in those specialties that make more money for the hospital, not in primary care, and certainly not in rural tracks (Primary Care and Residency Expansion, January 7, 2010 ). As they expand, in response to the demand for more physicians and medical school class increases, they will exert great political pressure to have new GME slots assigned to them to help cover their costs.
So here is the situation:
· There is a tremendous shortage of doctors in rural areas.
· Rural family medicine training programs, particularly those located in rural areas, are very effective in producing physicians who will practice in those rural underserved areas.
· Only 7.3% of family medicine (FM) residency positions are in such rural programs. This is way better than any other specialty, and may in fact be higher because while the authors did not count many of the trainees claimed as rural by urban FM residencies because they are not actually occurring in RUCA-defined rural areas, “Training locations may be defined as 'urban' using RUCA definitions but may still be sparsely populated and serve a predominantly rural patient populations.”
· Even if all FM positions claimed by their sponors as rural are in fact so, FM residents are only about 10% of all residency positions (2,630 of 25,500 in 2010), and virtually no other residents are trained for, not to mention likely to enter, rural practice…despite the need for other specialists, especially general surgeons, in these communities.
· ACA has a number of components that target an increase in the production of rural physicians (particularly family doctors and general surgeons, Public Law 111-148, Sect 5501, p. 534), but even if these are fully implemented, and taken advantage of by students, it will be many years before they have a significant impact.
· Despite these ACA changes, there will be counterpressures to use many of the new training slots for training non-primary care residents in urban sites, and particularly in academic health centers; these will come from both the academic health centers and their teaching hospitals themselves, the subspecialty physician medical societies, and the medical students themselves who overwhelmingly prefer to live in urban areas, as well as to earn the much higher incomes of subspecialists.
How might this be changed or modified? The provisions in the ACA law funding of GME slots to non-hospital settings such as community health centers, preferentially training primary care doctors (and general surgeons), and supporting the growth of community health centers and health extension services are a start, but they are not sufficient. The key is going to be greater incomes for doctors practicing primary care and general surgery in rural areas compared to those practicing subspecialties in urban areas. Supply and demand is insufficient; while there is demand for such doctors in rural areas, there is demand for more subspecialists by urban hospitals that see them as cash cows. Medicare sets reimbursement rates, as almost all payers model their rates as percents (usually higher) of Medicare’s. The reimbursement has to change so dramatically as to make primary care doctors in rural areas make, if not more, at least not nearly so much less as subspecialists in cities.
This financial change will begin to level the playing field. Medical students who have no interest in rural practice can still stay in urban areas, and even in subspecialties, but they should have to pay a financial price, making less than they would if they were to practice in what (to them) might be considered a less desirable area. As long as we make some careers pay a lot more, often for no more or even less work, as well as be located more popular (urban metropolitan) areas, we cannot expect any different outcome from the one we currently have.
[1] Chen FM, Andrilla CHA, Doescher MP, Morris C, “Family Medicine Residency Training in Rural Locations”, Final Report #126, WWWAMI Rural Health Research Center, University of Washington School of Medicine Department of Family Medicine, July 2010.
[2] RUCA = Rural-Urban Commuting Areas; a measure of population density that accounts for nearness to an urban area; obviously two counties may have similarly low population densities, but if one is surrounded by similar counties while the other is adjacent to a county with a large – or moderate – urban area, the first is “more” rural.
[3] Morris CG, Chen FM, Training Residents in Community Health Centers: Facilitators and Barriers, Annals of Family Medicine, Nov2009;7(6):488-94
- Primary Care And Rural Areas
. "The primary care physician and health reform”,[1] by Robert H. Brook and Roy T. Young of the RAND Corporation, appears In the April 21, 2010 issue of JAMA. Rather than review the various components of the new Patient Protection and Affordable Care...
- Rural Pipelines Versus Long Term Obligations
Generic expansions nationwide can be expected to result in no change from the 9% of physicians found in rural areas. To few remain instate, choose needed locations, and remain instate in needed locations. Voluntary pipelines are still limited by lack...
- No Country For Health Care: Rural Medicine In America
Thanks to Dr. Fitzhugh Mullan and colleagues at the Medical Education Futures Study for letting me know about a terrific 4-part series of articles by Emily Ramshaw of the Texas Tribune. In "No Country for Health Care," Ramshaw documents the severe difficulties...
- Re-priming The Primary Care Pipeline
If you've been reading this blog since its inception, you are now well aware that primary care is essential to any high-performing health system, including those in other countries, but that the "pipeline" for primary care physicians in the U.S. has...
- Christmas Gift
On Christmas morning as we were opening presents with our kids and family, I got to thinking about how lucky I am. I really don't know how I got into medical school. I grew up in a pretty modest home. These days you would have called us poor. At...
Medicine
Training rural family doctors
.
In a recent report from the University of Washington’s WWAMI Rural Research Center, “Family Medicine Residency Training in Rural Locations”,[1] Chen et. al. repeat their 2000 study of rural training in the US. They note that this is very important given the health needs of the American people, 20% of whom live in rural areas, most of which are underserved given the less than 9% of doctors who practice there (Primary Care and Rural Areas, April 28, 2010; Medicare Costs in Rural America: A case of reaping what we haven't sown?, March 26, 2009). Most rural training is of family doctors, but a majority of it comes from urban programs.
How is this so? This is because over 90% of the family medicine residency programs in the nation are located in urban areas, and only 7% in “large rural areas”; it is very hard to have a program entirely in a “small rural area” as the requirements for family medicine training include a great deal of time spent in the hospital and working with other specialists. Nonetheless, the authors surveys discovered that nearly half of the family medicine programs felt that training rural doctors was an important part of their mission.
From the Executive Summary: “Rural residency programs provided a higher proportion of rural training than urban programs,
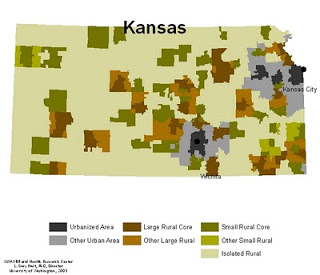 but because more programs were in urban settings, there was more rural training in urban than rural programs. Overall, 15% of respondents had a formal RTT [rural training track]; of these, 61% were in rural and 10% in urban programs. Rural residency programs conducted 83% of all rural residency training in RUCA[2]-defined rural areas. Comparing the 2000 and 2007 surveys, rural training increased from 372 to 408 FTEs, but rural training in urban programs declined from 186 to 79 FTEs, resulting in an overall decrease in the amount of rural-focused family medicine training.” See figure for example of a “RUCA map” in a state (Kansas) with a high percentage of “isolated rural” areas; Other states (say, New Jersey) look different!
but because more programs were in urban settings, there was more rural training in urban than rural programs. Overall, 15% of respondents had a formal RTT [rural training track]; of these, 61% were in rural and 10% in urban programs. Rural residency programs conducted 83% of all rural residency training in RUCA[2]-defined rural areas. Comparing the 2000 and 2007 surveys, rural training increased from 372 to 408 FTEs, but rural training in urban programs declined from 186 to 79 FTEs, resulting in an overall decrease in the amount of rural-focused family medicine training.” See figure for example of a “RUCA map” in a state (Kansas) with a high percentage of “isolated rural” areas; Other states (say, New Jersey) look different!The authors found that while virtually all (99.9%) of the training FTEs reported as rural in rural programs in fact occurred in rural (RUCA-defined) areas, only 21.7% of those reported by urban programs were in such areas. The net result was that only 7.3% of family medicine residency training FTEs are in rural areas, with 83% of these conducted by rural programs. Interestingly, to me, a higher percentage of urban programs listed rural training as “very important” (45.3%) than listed urban (underserved) training (40.4%).
The authors discuss the policy implications of this situation, including the possible impact of several components of the ACA health reform law that encourage training in rural areas. An important one has to do with Medicare funding of GME (residency) positions, the arcane but major source of funding for such training (Funding Graduate Medical Education, May 25, 2009; Public Law 111-148, Sect 5506, p 661). The change would make it easier for non-hospital sponsors of training (such as community health centers, an area the authors have also written about[3]) to receive this funding (Public Law 111-148, Sect 5508, p.668). The law – and policy – also favors redistribution of unfilled GME spots to rural hospitals. However, there are counterpressures: many big urban hospital training sites are “over their cap”, meaning they have more residency positions than are funded by Medicare. In these cases, the hospital, or another entity, funds the positions; these are virtually always in those specialties that make more money for the hospital, not in primary care, and certainly not in rural tracks (Primary Care and Residency Expansion, January 7, 2010 ). As they expand, in response to the demand for more physicians and medical school class increases, they will exert great political pressure to have new GME slots assigned to them to help cover their costs.
So here is the situation:
· There is a tremendous shortage of doctors in rural areas.
· Rural family medicine training programs, particularly those located in rural areas, are very effective in producing physicians who will practice in those rural underserved areas.
· Only 7.3% of family medicine (FM) residency positions are in such rural programs. This is way better than any other specialty, and may in fact be higher because while the authors did not count many of the trainees claimed as rural by urban FM residencies because they are not actually occurring in RUCA-defined rural areas, “Training locations may be defined as 'urban' using RUCA definitions but may still be sparsely populated and serve a predominantly rural patient populations.”
· Even if all FM positions claimed by their sponors as rural are in fact so, FM residents are only about 10% of all residency positions (2,630 of 25,500 in 2010), and virtually no other residents are trained for, not to mention likely to enter, rural practice…despite the need for other specialists, especially general surgeons, in these communities.
· ACA has a number of components that target an increase in the production of rural physicians (particularly family doctors and general surgeons, Public Law 111-148, Sect 5501, p. 534), but even if these are fully implemented, and taken advantage of by students, it will be many years before they have a significant impact.
· Despite these ACA changes, there will be counterpressures to use many of the new training slots for training non-primary care residents in urban sites, and particularly in academic health centers; these will come from both the academic health centers and their teaching hospitals themselves, the subspecialty physician medical societies, and the medical students themselves who overwhelmingly prefer to live in urban areas, as well as to earn the much higher incomes of subspecialists.
How might this be changed or modified? The provisions in the ACA law funding of GME slots to non-hospital settings such as community health centers, preferentially training primary care doctors (and general surgeons), and supporting the growth of community health centers and health extension services are a start, but they are not sufficient. The key is going to be greater incomes for doctors practicing primary care and general surgery in rural areas compared to those practicing subspecialties in urban areas. Supply and demand is insufficient; while there is demand for such doctors in rural areas, there is demand for more subspecialists by urban hospitals that see them as cash cows. Medicare sets reimbursement rates, as almost all payers model their rates as percents (usually higher) of Medicare’s. The reimbursement has to change so dramatically as to make primary care doctors in rural areas make, if not more, at least not nearly so much less as subspecialists in cities.
This financial change will begin to level the playing field. Medical students who have no interest in rural practice can still stay in urban areas, and even in subspecialties, but they should have to pay a financial price, making less than they would if they were to practice in what (to them) might be considered a less desirable area. As long as we make some careers pay a lot more, often for no more or even less work, as well as be located more popular (urban metropolitan) areas, we cannot expect any different outcome from the one we currently have.
[1] Chen FM, Andrilla CHA, Doescher MP, Morris C, “Family Medicine Residency Training in Rural Locations”, Final Report #126, WWWAMI Rural Health Research Center, University of Washington School of Medicine Department of Family Medicine, July 2010.
[2] RUCA = Rural-Urban Commuting Areas; a measure of population density that accounts for nearness to an urban area; obviously two counties may have similarly low population densities, but if one is surrounded by similar counties while the other is adjacent to a county with a large – or moderate – urban area, the first is “more” rural.
[3] Morris CG, Chen FM, Training Residents in Community Health Centers: Facilitators and Barriers, Annals of Family Medicine, Nov2009;7(6):488-94
- Primary Care And Rural Areas
. "The primary care physician and health reform”,[1] by Robert H. Brook and Roy T. Young of the RAND Corporation, appears In the April 21, 2010 issue of JAMA. Rather than review the various components of the new Patient Protection and Affordable Care...
- Rural Pipelines Versus Long Term Obligations
Generic expansions nationwide can be expected to result in no change from the 9% of physicians found in rural areas. To few remain instate, choose needed locations, and remain instate in needed locations. Voluntary pipelines are still limited by lack...
- No Country For Health Care: Rural Medicine In America
Thanks to Dr. Fitzhugh Mullan and colleagues at the Medical Education Futures Study for letting me know about a terrific 4-part series of articles by Emily Ramshaw of the Texas Tribune. In "No Country for Health Care," Ramshaw documents the severe difficulties...
- Re-priming The Primary Care Pipeline
If you've been reading this blog since its inception, you are now well aware that primary care is essential to any high-performing health system, including those in other countries, but that the "pipeline" for primary care physicians in the U.S. has...
- Christmas Gift
On Christmas morning as we were opening presents with our kids and family, I got to thinking about how lucky I am. I really don't know how I got into medical school. I grew up in a pretty modest home. These days you would have called us poor. At...
